increasing of black fungus during pandemic
black fungus
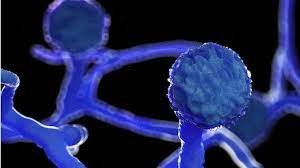
What is Black Fungus?
Black fungus, or mucormycosis, is a complication caused by a fungal infection. This is a relatively rare but potentially fatal condition.
what is white fungus?
Like the black fungus, white fungus is also more likely to afflict people with compromised immune systems, pre-existing medical conditions, AIDS, a recent kidney transplant or diabetes, experts say.

What is Mucormycosis Disease?
it's a fungal disease.we are not familier with this diseases. normally we are not infected with the diseases. when someone have low immunity power to fight with the bacteria,virus and many others germs in the environment then this fungus can nest in human body.
Fungus infected status in india
In the past few weeks, thousands of black fungus cases have been reported across the country, with hundreds hospitalized and at least 90 dead. Two states have declared it an epidemic, and the central government has made it a notifiable disease.
Amid the rising cases of Black Fungus infection in several states of India, four cases of White Fungus infection have been reported from Patna in Bihar. It is to be noted that White Fungus is considered more dangerous than Black Fungus. One of the infected patients is a famous doctor from Patna.
What types of infection do these fungi cause?
Generally, some types of fungi don’t cause any infections in humans but can cause sickness in people with weakened immune systems known as opportunistic infections.
Some common types of a fungal infection include:
1.Skin infections like ringworm
2.Nail infections
3.Deeper cutaneous infections following trauma,
4.Breach in the skin with subsequent fungal implantation and growth
5.Sinus infections and deep lung infections
6.The fungi can also affect the gastrointestinal system, renal systems and can cause a full-blown infection resulting from the entry of fungus into the bloodstream.
Symptoms of Mucormycosis
The symptoms of mucormycosis depend on where in the body the fungus is growing. Contact your healthcare provider if you have symptoms that you think are related to mucormycosis.
Symptoms of rhinocerebral (sinus and brain) mucormycosis include:
- One-sided facial swelling
- Headache
- Nasal or sinus congestion
- Black lesions on nasal bridge or upper inside of mouth that quickly become more severe
- Fever
Symptoms of pulmonary (lung) mucormycosis include:
- Fever
- Cough
- Chest pain
- Shortness of breath

why is it occurring in COVID 19 patients?
Mucormycosis can occur any time after COVID-19 infection, either during the hospital stay or several days to a couple of weeks after discharge.
“The COVID-19 causes favourable alteration in the internal milieu of the host for the fungus and the medical treatment given, unwittingly also abets fungal growth. COVID-19 damages the airway mucosa and blood vessels. It also causes an increase in the serum iron which is very important for the fungus to grow. Medications like steroids increase blood sugar. Broad-spectrum antibiotics not only wipe out the potentially pathogenic bacteria but also the protective commensals. Antifungals like Voriconazole inhibit Aspergillosis but Mucor remains unscathed and thrives due to lack of competition. Long-term ventilation reduces immunity and there are speculations of the fungus being transmitted by the humidifier water being given along with oxygen. All the above make for a perfect recipe for mucormycosis infection,” he explained.

Are these infections life-threatening?
These infections are very lethal, and if not treated most will not make it. The mortality ranges between 25 to 90%. Once the infection spreads into the brain mortality is very high. Hence a lot of importance is given to early diagnosis and prompt institution of treatment.
How do you treat it?
How to prevent the occurrence of fungus?
Prevention is always better than cure.
In hospital:
*Maintenance of good hygiene and cleanliness is a must. Regular oral hygiene care with mouthwash, povidone-iodine gargles must be done.
*While administering oxygen, water for humidification must be sterile and there should be no leakage from the humidifier.
*Steroid usage must be limited to no more than necessary with strict blood glucose control.
*Unnecessary use of broad-spectrum antibiotics, antifungals should not do as this removes the normal commensal flora resulting in the growth of unwanted organisms due to lack of competition.
Once discharged:
*Stay indoors as much as possible
*Regular exercises
*Control of blood sugars
*At home, the surroundings must be clean and free from dust and dampness
*Maintain oral and nasal hygiene
*While going out always wear an N-95 mask
*Avoid construction areas, fields, grounds.
*Soil and plants are the areas that abound with fungi. Hence better to avoid working with soil, gardening. If unavoidable, masks, rubber gloves, and boots are a must.